Quality of Care in India
In the National Health Policy 2017, India committed to reduce maternal mortality ratio (MMR) to 100 per 100 000 live births by 2020, under 5 mortality to 23 per 1000 live births by 2025, infant and neo-natal mortality to 16 per 1000 live births and still birth rate to “single digit” by 2025.
National Leadership
Several initiatives were launched to address key gaps in care for pregnant mothers and to accelerate reductions in maternal and newborn mortality. In 2016, Pradhan Mantri Surakshit Matritva Abhiyan (PMSMA) was launched to target the needs of pregnant mothers for quality antenatal examinations. Under PMSMA, doctors in both the public and private sector examine expecting mothers on the 9th day of each month. In 2017, the Labor Room and maternity Quality Improvement Initiative (LaQshya) launched to improve the quality of intrapartum and immediate post-partum care provisions in public facilities. LaQshya is an ambitious national initiative focused on improving the positive birthing experience and respectful maternity care for all women attending public health institutions. LaQshya is being scaled up nationwide, and implementation involves improving infrastructure upgrades, ensuring the availability of essential equipment, providing adequate human resources, capacity building of health care workers and provision of ongoing quality improvement support to health facilities. The Maternal and Newborn Health (MNH) Toolkit that was first developed in 2015 has been expanded to include guidelines for establishing obstetric intensive care unit (ICU). This provide guidance for sub-district level health facilities and district level hospitals and was revised in 2021 to respond to the context of the COVD-19 pandemic.
In 2019, the Ministry of Health and Family Welfare, India launched the Surakshit Matritva Aashwasan (SUMAN) initiative which aims to provide assured, dignified, respectful and quality healthcare, at no cost and zero tolerance for denial of services, for every woman and newborn. The initiative aims to achieving zero preventable maternal and neonatal mortality and to provide high quality services in public facilities. This comprehensive initiative provides service guarantee, a responsive client feedback and grievance redressal mechanism, community linkages and support systems and 100 percent reporting for maternal and infant deaths.
During 2022, the Ministry of Health and Family Welfare has been prioritizing the adaptation of the WHO Standards for improving the quality of care for children and young adolescents in health facilities and development of a roadmap for the roll out of Quality Improvement (QI) standards for newborn and child health. A National Quality Improvement initiative for developing child friendly services in public health facilities (MusQan) was launched in 2021.
In 2018, the Government of India took the landmark policy decision to roll out midwifery services in the country to improve the quality of care of maternity services, ensure task shifting among the health personnel and ensure respectful care to pregnant women and newborns.
Efforts to systemize Maternal and Perinatal Death Surveillance and Review (MPDSR) at national level and improve reporting of maternal and perinatal deaths were identified as key priorities for 2022. The online integrated information system notification and surveillance on MPDSR is being scaled up and strengthened at national level. Discussions with the Federation of Obstetric and Gynecological Societies of India (FOGSI) were initiated in 2022 on improving reporting of MPDSR and ensuring auditing systems are in private sector facilities.
To improve the quality of maternal and newborn services in private facilities, ‘Manyata’ a certification programme with both quality improvement and assurance components was established in 2013. Manyata’s approach is to develop a successful public-private partnership for quality of care. Since its launch, Manyata has developed a viable business model for quality assurance and laid the groundwork for sustainable quality improvement efforts in the private maternal health care sector in India. The programme is implemented in a number of States; Uttar Pradesh, Jharkhand and Maharashtra by Jhpiego and in Rajasthan, Karnataka and Tamil Nadu by other partners. Work is ongoing at national level to strengthen private sector facilities and engagement in quality-of-care initiatives including work with Manyata team and Merck for Mothers on private sector engagement for quality of care.
District and Facility Quality Improvement
The WHO South-East Asia Regional Office (SEARO) model of Point of Care Quality Improvement (POCQI) is being implemented nationwide. This model aims to improve the quality of care at the very point the patient comes in contact with a healthcare worker. Although challenges presented to scale -up the quality of care intervention to additional sites during the COVID-19 pandemic, India continued to train healthcare workers and build capacities for the implementation of POCQI. Online POCQI and QI workshops were held in 2021 to introduce the four basic steps of POCQI and catalyze quality of care for maternal and newborn care. To adapt to the new context, a e-learning POCQI workbook was developed. A Training of Trainers workshop was held in 2021 which aimed to upskill the enthusiastic QI champions from the already trained pool of participants of Nationwide Quality of Care Network (NQOCN). In 2022, India plans to integrate POCQI in undergraduate and postgraduate university programmes; the Indian Institute of Health Management and Research and WHO are working to integrate the modules on Point of Care Quality Improvement (POCQI) in academic and training programs for public health professionals. The course will serve to train future public health professionals on using PoCQI methodologies for undertaking quality improvement initiatives.
In order to ensure QI teams are sharing their experiences and lessons on QI, the Nationwide Quality of Care Network (NQOCN) was established in 2017. This is voluntary network of teams - a community of practice - working on quality improvement initiatives across 15 States in India. The Network aims to empower healthcare workers to continuously improve quality of care, encourage community participation in the QI process and create a culture of QI in the healthcare system. This Network also facilitates cross-learning and experience sharing across QI teams, for example a community of practice was also recently developed to share knowledge and experience in the implementation of the POCQI model.
As part of efforts to evaluate the implemented QI programs, capacity building and trainings of RMNCH program managers were conducted at national level in 2022. "Managing programs on reproductive, maternal, newborn, child and adolescent health" is a modular-based training designed to build capacity of program managers to effectively deliver evidence-based interventions. The National Training of Trainers was conducted in June 2022 and regional trainings for aspirational Districts (with low performance on key RMNCAH indicators) in high burden states will be initiated in 2023.
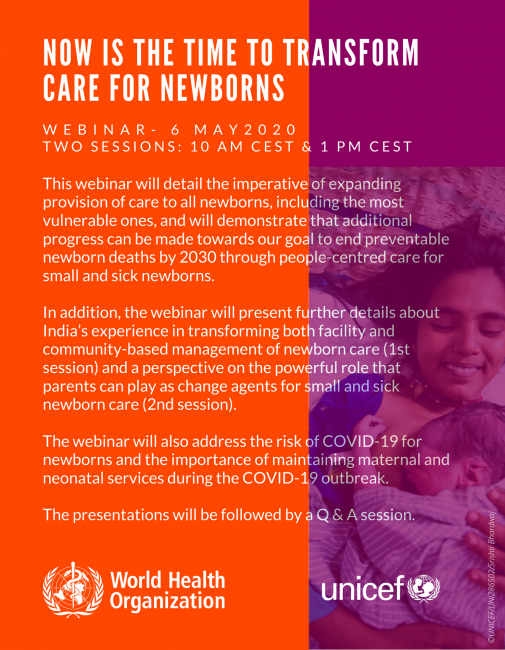
Photo: Bindu Devi with her son Sahil Kumar at the Bhagwanpuri Raiti village Anganwadi health clinic in Bihar, India, in June 2010. ©UNICEF/Graham Crouch